It’s common for patients to ignore the early warning signs of neuropathy, assuming that tingling or numbness in the feet is “just poor circulation” or something temporary. However, untreated neuropathy can progress over time and lead to serious complications.
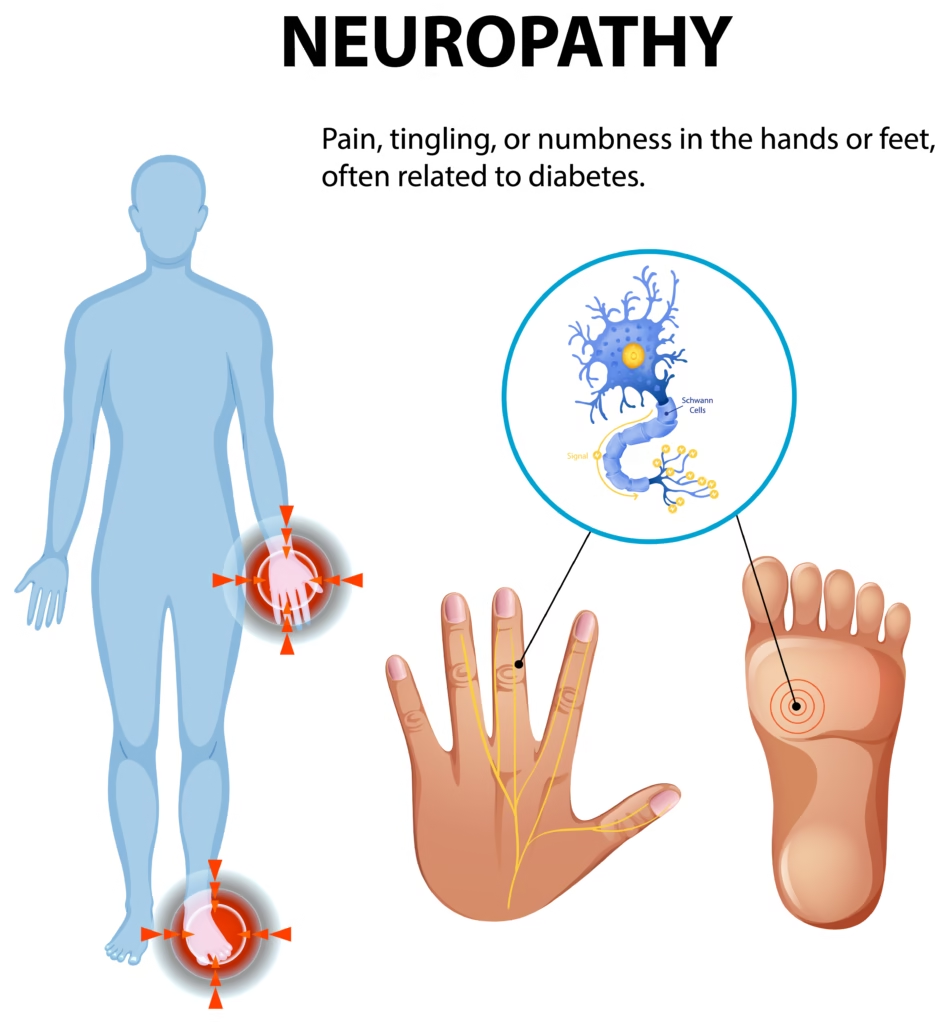
Table of Contents
Introduction
Understanding Nerve Health
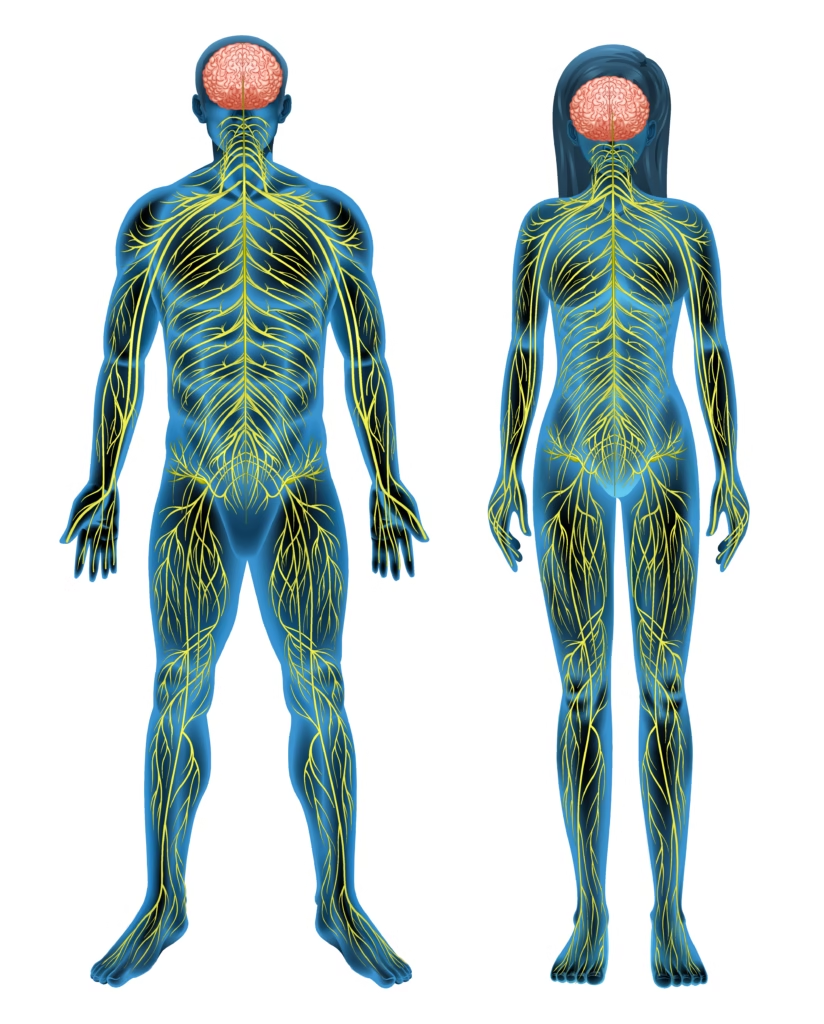
As your doctor, I want you to understand that your nervous system is one of the most complex and important parts of your body. Nerves act like electrical wires, carrying messages from your brain and spinal cord to the rest of your body. When these wires are healthy, signals move quickly and accurately. But when nerves are damaged, those signals may be slowed, altered, or even blocked. This condition is called neuropathy.
Neuropathy is not a single disease—it is a medical term we use when nerves are injured or malfunctioning. It may affect just one nerve, a group of nerves, or many nerves throughout your body. Because nerves control so many functions—movement, sensation, digestion, blood pressure, and even sweating—neuropathy can present in many different ways.
For some, it begins as a tingling or numbness in the feet. For others, it may show up as burning pain in the hands, weakness in the legs, or even digestive issues. My goal in this article is to explain neuropathy in simple terms so you can recognize its early signs, understand its causes, and know what treatment options are available.
Why Neuropathy Deserves Attention
It’s common for patients to ignore the early warning signs of neuropathy, assuming that tingling or numbness in the feet is “just poor circulation” or something temporary. However, untreated neuropathy can progress over time and lead to serious complications.
When sensory nerves are affected, you may not feel injuries to your feet or hands. A small blister could turn into a large infection if unnoticed, especially in patients with diabetes. Neuropathy can also weaken muscles, making it harder to walk or maintain balance, which increases your risk of falls.
If the autonomic nerves are involved, symptoms may include dizziness when standing, changes in digestion, bladder problems, or irregular heartbeat. These complications highlight why neuropathy is more than just a discomfort—it can affect your independence and overall health if not managed properly.
As your physician, I encourage you not to dismiss early signs. The sooner neuropathy is identified, the better we can manage symptoms, slow its progression, and maintain your quality of life.
Types of Neuropathy
Peripheral Neuropathy
The most common form of neuropathy is peripheral neuropathy, which affects the nerves in your extremities—most often the feet and hands. Patients usually describe it as tingling, burning, or “pins and needles.” Some say it feels like walking on cotton, while others experience sharp, stabbing pain that can make even light touch from socks or shoes uncomfortable.
Over time, numbness may set in. While you might think numbness is preferable to pain, it actually increases the risk of injuries going unnoticed. For example, if you step on a small object or develop a blister, you might not feel it. Left untreated, such injuries can lead to infections, especially in those with diabetes.
Peripheral neuropathy can also affect motor nerves, leading to muscle weakness and difficulty with coordination. Patients sometimes find that they drop objects more often or struggle with simple tasks like buttoning a shirt.
Autonomic Neuropathy
Autonomic nerves control involuntary functions—things your body does automatically, without you having to think about them. When these nerves are affected, symptoms can be wide-ranging and sometimes confusing.
You may notice problems with digestion, such as bloating, nausea, constipation, or diarrhea. Some patients experience bladder dysfunction, either difficulty emptying or frequent urgency. Others may notice changes in sweating, either excessive sweating or very little at all.
One particularly concerning symptom is dizziness or fainting when standing up quickly, caused by unstable blood pressure. Because autonomic neuropathy involves critical body systems, it often requires careful evaluation and tailored treatment.
Proximal Neuropathy
Proximal neuropathy is less common but can be very painful. It affects nerves in the thighs, hips, or buttocks and usually occurs in older adults, particularly those with diabetes. Patients often describe sudden, severe pain in one leg, followed by weakness that makes it difficult to rise from a seated position or climb stairs.
This type of neuropathy may improve over time, but recovery can take months. In the meantime, physical therapy and pain management are essential. Patients should not ignore sudden, severe pain or weakness in the legs, as early intervention improves outcomes.
Focal Neuropathy
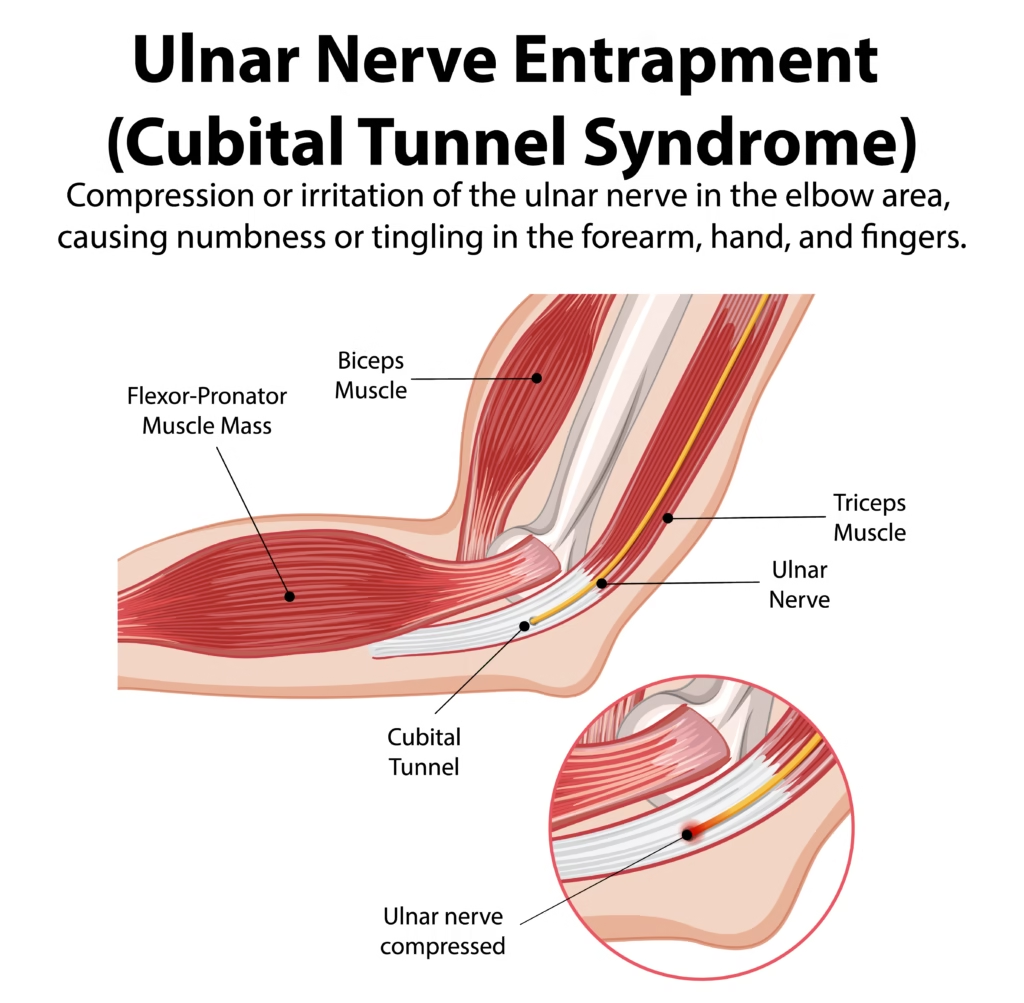
Focal neuropathy develops when a single nerve or small group of nerves is affected. Unlike peripheral neuropathy, which spreads gradually, focal neuropathy appears suddenly.
It can cause double vision, facial weakness (such as Bell’s palsy), or sharp pain in specific areas of the body like the chest or abdomen. Because its symptoms mimic other conditions, it can be alarming for patients. The good news is that focal neuropathy often improves on its own within weeks to months.
Still, medical evaluation is essential to rule out other serious conditions and to provide supportive treatment if needed.

Common Causes of Neuropathy
Diabetes and Nerve Damage
Among all the possible causes, diabetes is the most frequent contributor to neuropathy worldwide. High blood sugar over time damages the tiny blood vessels that supply oxygen and nutrients to nerves. Without proper nourishment, nerves lose their ability to function, leading to diabetic neuropathy.
Diabetic neuropathy often begins in the feet, with symptoms like tingling, burning, or numbness. Over time, it may progress to the legs and hands. Because diabetes also impairs circulation and wound healing, patients with diabetic neuropathy are at high risk for foot ulcers and infections.
Good blood sugar control is the most important step in prevention. Regular foot exams, proper footwear, and early treatment of minor injuries are also critical for avoiding complications.
Alcohol and Lifestyle Factors
Excessive alcohol intake can directly damage nerve tissue, leading to alcoholic neuropathy. Patients may notice numbness, tingling, or weakness in their hands and feet. Alcohol abuse also contributes to poor nutrition, especially deficiencies in B vitamins, which are essential for nerve health.
Other lifestyle factors, such as smoking, can worsen neuropathy by reducing blood flow to the nerves. Patients are strongly advised to reduce or eliminate alcohol and tobacco use to protect nerve.

Vitamin Deficiencies and Malnutrition
Your nerves depend on certain vitamins to function properly, especially the B vitamins—B1, B6, B12, and folate. When these are lacking, nerve signals can slow down or become disrupted, leading to neuropathy. Vitamin B12 deficiency, in particular, is a common cause of nerve damage. Patients often describe numbness in the feet, unsteady walking, and memory problems when B12 levels are too low.
Deficiency can occur due to poor diet, digestive conditions (like pernicious anemia or celiac disease), or long-term use of certain medications such as acid reflux drugs (proton pump inhibitors) or metformin. Malnutrition—whether from chronic illness, eating disorders, or excessive alcohol use—also raises the risk.
The good news is that vitamin-related neuropathy can often be reversed if detected early. Blood tests can confirm deficiencies, and treatment may involve dietary changes, oral supplements, or injections. This is why I always encourage my patients to maintain a balanced diet rich in lean proteins, whole grains, leafy greens, and fortified foods.

Autoimmune Conditions and Infections
Your immune system is designed to protect you, but in some cases, it mistakenly attacks healthy nerves. Conditions like lupus, rheumatoid arthritis, Guillain-Barré syndrome, and multiple sclerosis can trigger nerve inflammation and damage, leading to neuropathy. These cases can be unpredictable, and flare-ups may worsen symptoms suddenly.
Infections can also play a role. Viruses such as shingles, HIV, or hepatitis C may damage nerves directly or set off an autoimmune response that harms them. Bacterial infections like Lyme disease and leprosy are also well-known causes of neuropathy in certain parts of the world.
Managing neuropathy caused by autoimmune disease or infection usually involves treating the underlying condition. For example, antiviral or antibiotic therapy may help with infection-related neuropathy, while immunosuppressive medications may be needed for autoimmune conditions.
Medications and Toxins
Certain medications, especially chemotherapy drugs, are known to cause neuropathy. This is often called chemotherapy-induced peripheral neuropathy (CIPN). Patients undergoing cancer treatment sometimes notice tingling, numbness, or burning sensations in their hands and feet that may persist even after treatment ends.
Other medications, including some used for blood pressure, infections, and autoimmune conditions, may also contribute to nerve damage. Environmental toxins such as heavy metals (lead, mercury, arsenic) can have similar effects.
If you ever notice nerve-related symptoms after starting a new medication, it is important to discuss it with your doctor immediately. Never stop a prescribed medication on your own, but do let us know—sometimes we can adjust the dosage, change the drug, or recommend supportive therapies to protect your nerves.

Early Symptoms and Warning Signs
Tingling and Numbness
One of the earliest signs of neuropathy is a tingling sensation, often starting in the toes or fingertips. Patients sometimes describe it as a “pins and needles” feeling or a mild buzzing under the skin. Over time, tingling may progress to numbness, where you lose the ability to feel pressure, temperature, or even pain in the affected areas.
While this may seem harmless at first, numbness increases the risk of unnoticed injuries. For example, a small cut or blister on the foot can become infected if you don’t feel it right away. This is why I encourage my patients with diabetes or neuropathy symptoms to perform daily foot checks.
Pain Patterns and Sensations
Neuropathy pain varies widely. Some patients describe sharp, stabbing pain, while others report burning or shooting sensations. A common complaint is that pain worsens at night, disrupting sleep.
In certain cases, even light touch—like bedsheets brushing against the skin—can trigger discomfort. This heightened sensitivity, called allodynia, is particularly frustrating because ordinary sensations become painful.
Keeping a journal of your pain patterns—when they occur, what triggers them, and what brings relief—can help your doctor design a more effective treatment plan.
Muscle Weakness and Balance Problems
When motor nerves are affected, neuropathy can cause muscle weakness. Patients may find it harder to grip objects, climb stairs, or stand up from a seated position. Over time, this weakness can contribute to poor posture, joint strain, and fatigue.
Another major concern is balance. Because nerves in your feet send signals to your brain about position and movement, damaged nerves can make you feel unsteady or cause frequent falls. For older adults, this significantly increases the risk of fractures and long recovery times.
Physical therapy, balance training, and regular exercise play a big role in preventing complications from neuropathy-related weakness.
Sensitivity to Touch and Temperature
Nerve damage can distort your ability to sense temperature changes. Some patients lose sensitivity and may not realize they are stepping into very hot water, leading to burns. Others may develop extreme sensitivity, where even mild heat or cold feels painful.
This is why I caution patients with neuropathy to always check bath water with their elbow before stepping in and to avoid using heating pads directly on the skin. Protecting your skin from unnoticed injuries is an essential part of neuropathy care.

How Neuropathy is Diagnosed
Clinical Examination and Medical History
The first step in diagnosing neuropathy is a detailed discussion of your symptoms and medical history. I’ll ask about the onset, pattern, and severity of your symptoms, as well as any medical conditions, medications, or family history that may contribute.
During the physical exam, I’ll test reflexes, muscle strength, and sensation. Simple tools such as a tuning fork, monofilament (a thin nylon fiber), or pinprick may be used to check how well your nerves respond to different types of stimulation.
Laboratory Investigations
Blood tests can provide valuable information about possible underlying causes. We may check for:
- Blood sugar levels (to assess for diabetes or prediabetes)
- Vitamin deficiencies, especially B12
- Thyroid function
- Signs of infection or autoimmune disease
In some cases, additional tests may be needed to look for toxins, kidney disease, or liver problems that could contribute to nerve damage.
Nerve Function Tests
Specialized tests help us measure how well your nerves are working:
- Nerve conduction studies (NCS): Small electrical pulses are delivered to the nerves to see how quickly signals travel.
- Electromyography (EMG): A thin needle electrode is inserted into muscles to record electrical activity. This helps determine whether weakness is caused by nerve or muscle problems.
These tests may sound intimidating, but they provide precise information that guides treatment planning.
Importance of Early Detection
Catching neuropathy early gives us the best chance to slow or even halt its progression. The earlier we identify nerve damage, the more treatment options are available. For example, if caught early, controlling blood sugar or correcting vitamin deficiencies can prevent long-term damage.
Delaying evaluation often means symptoms have already advanced, making them harder to manage. That’s why I encourage patients not to wait—if you notice persistent tingling, numbness, or unexplained weakness, it’s time to schedule a visit.
Treatment Options for Neuropathy
Medications for Pain Management
While there is no single cure for neuropathy, we do have medications that can help manage the pain and discomfort. Over-the-counter options like acetaminophen or ibuprofen may provide relief for mild cases, but for persistent or severe neuropathy, prescription medicines are often necessary.
Some of the most effective medications belong to classes not traditionally used for pain, such as:
- Antidepressants (e.g., amitriptyline, duloxetine): These can help regulate how the brain processes pain signals.
- Anticonvulsants (e.g., gabapentin, pregabalin): Originally developed for seizures, these medicines calm overactive nerves.
- Topical treatments (capsaicin cream, lidocaine patches): Useful for localized nerve pain in areas like the feet or hands.
For more severe cases, stronger pain relievers may be considered, but we use them cautiously because of the risk of dependence. The goal is to strike a balance: enough medication to keep you comfortable, but not so much that you face unnecessary side effects.
Physical Therapy and Exercise
Movement is medicine for your nerves. Physical therapy plays a major role in maintaining strength, flexibility, and balance. Specific exercises can help retrain weakened muscles, improve coordination, and reduce the risk of falls.
Gentle activities such as walking, swimming, or cycling improve circulation and promote nerve health. Stretching exercises can also reduce stiffness and improve mobility. In my practice, I often recommend working with a physical therapist, especially for patients with muscle weakness or significant balance issues.
The key is consistency. Even light activity, done regularly, can make a meaningful difference in slowing progression and improving overall function.

Lifestyle Changes and Diet Adjustments
Your daily habits have a powerful impact on nerve health. The following steps are especially important:
- Control blood sugar: For diabetic patients, this is the single most important factor in preventing worsening neuropathy.
- Balanced diet: Eat plenty of vegetables, whole grains, lean proteins, and foods rich in B vitamins.
- Avoid alcohol and smoking: Both worsen nerve damage and interfere with healing.
- Foot care: Inspect your feet daily, wear well-fitted shoes, and seek medical help for any wounds or infections immediately.
These may seem like small steps, but over time they protect your nerves and help prevent complications.
Surgical and Advanced Treatment Options
In some cases, when neuropathy is caused by nerve compression—such as carpal tunnel syndrome—surgical intervention may be considered to relieve pressure. For severe pain that does not respond to other treatments, advanced therapies like nerve stimulation (spinal cord stimulation or peripheral nerve stimulation) may be options.
These treatments are not suitable for everyone, but they can be life-changing for patients with chronic, disabling pain. The decision is always made after careful evaluation and discussion of risks and benefits.
Home and Natural Remedies
Herbal Supplements and Vitamins
Some patients benefit from supplements, though they should always be discussed with a doctor before use. Commonly considered options include:
- Alpha-lipoic acid: An antioxidant that may help reduce nerve pain, particularly in diabetic neuropathy.
- B vitamins: Essential for nerve repair and function.
- Acetyl-L-carnitine: May support nerve regeneration in certain cases.
While supplements can be supportive, they should not replace prescribed medical treatment.
Stress Management and Relaxation Techniques
Chronic pain often worsens with stress. Techniques like meditation, deep breathing, and yoga can help lower stress levels and reduce the intensity of symptoms. Patients who practice relaxation techniques regularly often report better sleep and improved coping abilities.
Acupuncture and Alternative Therapies
Some patients find relief through alternative approaches such as acupuncture. While research results are mixed, many patients report improvement in pain and circulation. Massage therapy and chiropractic care may also provide temporary relief, though they should be performed by trained professionals familiar with neuropathy care.
Preventing Neuropathy Progression
Blood Sugar Control for Diabetics
For diabetic patients, keeping blood sugar within the target range is the most effective way to prevent neuropathy from worsening. This includes following prescribed medications, regular glucose monitoring, and adhering to a diabetes-friendly diet.
Healthy Lifestyle and Balanced Diet
Maintaining a healthy weight, exercising regularly, and eating a nutrient-rich diet are important for everyone, not just diabetics. These habits improve blood flow, reduce inflammation, and provide the vitamins and minerals your nerves need to stay healthy.
Regular Exercise and Foot Care
Exercise not only strengthens muscles and improves balance but also stimulates nerve repair and blood circulation. Simple daily routines—like a 20-minute walk—can make a difference.
Foot care remains crucial. Patients with neuropathy should check their feet daily for cuts, blisters, or infections. I often remind my patients: “A small wound ignored today could be a major complication tomorrow.” Proper footwear and regular podiatry visits are essential preventive steps.
Living Well with Neuropathy
Coping with Daily Challenges
Neuropathy can interfere with simple activities like walking, cooking, or sleeping. Adaptive tools, such as supportive shoes, walking aids, or even specialized kitchen utensils, can help maintain independence. Occupational therapy may also provide strategies to make daily tasks easier and safer.
Emotional and Mental Health Support
Living with chronic pain takes a toll emotionally as well as physically. Many patients struggle with anxiety, depression, or frustration. I encourage my patients to seek support—not only from medical professionals but also from family, friends, and counselors. Mental health care is just as important as physical care.
Support Groups and Resources
Sometimes, the best comfort comes from talking to others going through the same challenges. Neuropathy support groups, whether in-person or online, provide encouragement, practical tips, and a sense of community.
As your doctor, I see firsthand how valuable these connections can be. You don’t have to face neuropathy alone—support and resources are available.
Conclusion
Neuropathy is a condition that deserves attention, not only because of the pain it causes but also because of the long-term risks it carries. While there is no single cure, early diagnosis, proper treatment, and lifestyle changes can make a significant difference in controlling symptoms and preserving quality of life.
If you notice early signs—tingling, numbness, or unexplained weakness—don’t wait. Talk to your doctor, get tested, and start treatment as soon as possible. With the right care, neuropathy can be managed, and you can continue living a full and active life.
FAQs
1. What foods should you avoid if you have neuropathy?
Patients should avoid excessive sugar, refined carbohydrates, alcohol, and processed foods that contribute to inflammation and poor blood sugar control.
2. Can neuropathy be completely cured?
In some cases, such as neuropathy caused by vitamin deficiencies or certain infections, symptoms can improve or even resolve with treatment. However, most types are managed rather than fully cured.
3. How long does it take for neuropathy to progress?
Progression varies. In diabetic patients with poor sugar control, symptoms may worsen quickly, while in others, progression may be slow and gradual.
4. Is neuropathy life-threatening?
Neuropathy itself is not usually life-threatening, but its complications—such as infections, falls, or heart rhythm issues from autonomic neuropathy—can be serious if untreated.
5. What is the best treatment for neuropathy pain?
The best treatment depends on the cause. Options include medications like pregabalin or duloxetine, physical therapy, and lifestyle changes. The key is an individualized plan designed with your doctor.

Well described in a structured and easy manner.