Fatty liver is becoming alarmingly common today—even among non-drinkers. As a doctor, I’ve seen countless patients struggle with this silent condition, but the good news is it’s completely reversible. Discover what causes fatty liver, why it’s rising so fast, and practical, doctor-approved steps to naturally reverse fatty liver and restore your liver health
Table of Contents
Introduction: Understanding Fatty Liver Disease
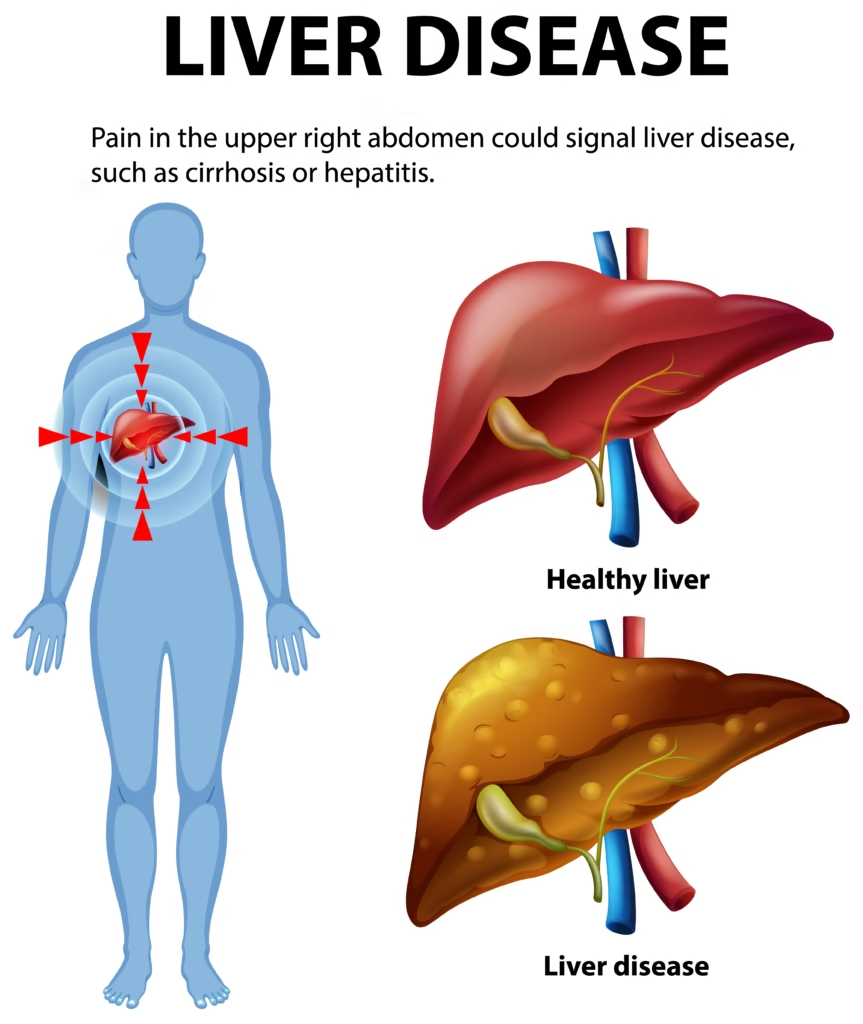
As a practicing doctor, I’ve noticed a concerning trend in recent years—a growing number of my patients are being diagnosed with fatty liver disease, and what’s even more alarming is that many of them have never touched alcohol in their lives. This condition, known as non-alcoholic fatty liver disease (NAFLD), is quietly becoming one of the most common liver problems across the world. Fatty liver occurs when excess fat builds up in the liver cells, leading to inflammation, scarring, and in severe cases, liver failure.
Our liver is a hardworking organ—it detoxifies the body, helps digest food, and regulates metabolism. But when fat starts accumulating, it’s like forcing a car engine to run with sludge inside it; it simply can’t function properly. In my clinic, I see patients from all walks of life—young professionals, homemakers, even teenagers—struggling with this “silent” disease. Most are shocked because they feel fine and have no symptoms, yet their liver enzymes and ultrasound reports tell a different story.
The good news is that fatty liver is reversible if diagnosed early and managed with the right lifestyle changes. In this article, I’ll walk you through what fatty liver is, why it’s becoming so common, and practical, science-backed ways to reverse it naturally—based on my experience treating patients over the years.
Why Fatty Liver Is Becoming So Common Today
When I began my medical career, fatty liver was something we usually associated with alcohol abuse. But over the past decade, I’ve seen a sharp rise in non-alcoholic fatty liver disease (NAFLD)—and it’s not limited to older adults. Even young adults in their 20s and 30s are showing fatty changes in the liver during routine health checkups. So, what’s driving this surge?
The answer lies in our modern lifestyle. We live in an era of sedentary habits, processed foods, and chronic stress. Most of us sit for long hours, snack on sugary or fried foods, and rely on fast food or packaged meals that are loaded with unhealthy fats and preservatives. Add to that irregular sleep patterns and little to no exercise, and the result is metabolic chaos—insulin resistance, obesity, and ultimately, fat deposition in the liver.
What’s even more concerning is that fatty liver often coexists with other health conditions like type 2 diabetes, high cholesterol, and high blood pressure. These are part of what we call metabolic syndrome, a dangerous cluster of conditions that significantly increase the risk of heart disease and stroke. Even in people who are not overweight, fatty liver can develop due to genetics, poor diet, or lack of physical activity.
In my clinic, I often tell patients that the liver is like a “silent worker”—it won’t complain until it’s under severe strain. So, prevention and early detection are key. The more we understand the causes, the better we can take charge of our liver health.
Difference Between Alcoholic and Non-Alcoholic Fatty Liver Disease (NAFLD)
Many patients come to me confused, saying, “Doctor, how can I have fatty liver when I don’t even drink alcohol?” That’s a fair question—and one I answer almost daily. There are two primary categories of fatty liver disease.
- Alcoholic Fatty Liver Disease (AFLD) – caused by excessive alcohol intake. Alcohol damages liver cells and leads to fat accumulation, inflammation, and scarring.
- Non-Alcoholic Fatty Liver Disease (NAFLD) – occurs in people who drink little to no alcohol but still have fat buildup in their liver.
NAFLD is now far more common than alcoholic fatty liver, especially in countries with increasing rates of obesity and diabetes. The primary culprits here are poor diet, insulin resistance, and lack of physical activity.
While both forms can progress to steatohepatitis (inflammation) and eventually cirrhosis (permanent liver scarring), the difference lies in the cause and management approach. In NAFLD, the focus is not on stopping alcohol but on improving metabolism, reducing weight, and making long-term lifestyle changes.
From my experience, when patients commit to consistent dietary improvements, moderate exercise, and better sleep, the liver starts to heal itself. It’s one of the few organs capable of regeneration—if given the right environment.

How Fatty Liver Develops in the Body
To truly understand how to reverse fatty liver, we must first know how it develops. Think of your liver as the body’s factory—it processes everything you eat, drink, and even breathe. When your body takes in more calories, especially from sugar and unhealthy fats, than it can use, the excess gets stored as fat. Some of this fat accumulates in the liver cells, leading to a condition called hepatic steatosis, or fatty liver.
In the beginning, this buildup might seem harmless, but over time, the liver becomes overloaded. The fat starts interfering with normal liver function, causing inflammation and oxidative stress. This inflammation damages liver cells and triggers the release of enzymes into the bloodstream—this is often when we first see elevated liver enzymes on blood tests.
The main driver of fatty liver, especially in non-alcoholic cases, is insulin resistance. When your cells stop responding properly to insulin, glucose levels rise, and the liver converts this excess sugar into fat. The result? More and more fat trapped inside liver cells.
It’s also worth noting that genetics can play a role—some people are predisposed to developing fatty liver even if they’re not overweight. But lifestyle remains the biggest factor. Sugary drinks, refined carbohydrates, fried foods, and prolonged sitting hours all worsen fat accumulation.
I often explain to my patients that a fatty liver doesn’t happen overnight—it’s the result of years of subtle, cumulative stress on the body. The good news, however, is that the same way the liver accumulated fat gradually, it can also shed that fat gradually—with consistent lifestyle and dietary changes.
Who Is at Risk? Common Causes and Risk Factors
When I sit across from a patient diagnosed with fatty liver, one of the first things I do is discuss their risk factors. Understanding why it happened is the first step toward reversing it. Here are the main contributors I commonly see in clinical practice:
- Obesity and Overweight – Carrying excess body fat, especially around the abdomen, significantly increases the risk of NAFLD.
- Type 2 Diabetes and Insulin Resistance – These conditions make it harder for the body to regulate blood sugar, pushing fat storage in the liver.
- High Cholesterol and Triglycerides – Elevated lipid levels contribute to fat deposition.
- Poor Diet – Diets high in processed foods, added sugars, and saturated fats promote liver fat accumulation.
- Lack of Physical Activity – A sedentary lifestyle slows metabolism and prevents the body from burning stored fat efficiently.
- Genetics – A family history of fatty liver or metabolic disorders can increase risk.
- Certain Medications – Some drugs, like corticosteroids or tamoxifen, can cause fatty changes in the liver.
It’s also surprising how “skinny fat” individuals—those who look thin but have high body fat percentages—can develop fatty liver too. I’ve treated several such patients who were shocked to find out they had liver fat despite a normal body weight. Their main issue was visceral fat—fat around internal organs caused by poor diet and lack of exercise.
Recognizing these risk factors early helps in prevention and management. If you have one or more of these risks, it’s crucial to get your liver enzymes and ultrasound checked periodically.
Symptoms of Fatty Liver: The Silent Warning Signs
Here’s the tricky part about fatty liver—it’s often silent in the early stages. Most people don’t feel anything unusual until the disease has already progressed. That’s why I always call it the “silent epidemic.”
Common early signs include:
- Persistent fatigue or lack of energy
- A feeling of heaviness or discomfort in the upper right abdomen
- Mild nausea or bloating
- Unexplained weight gain, especially around the belly
- Slight yellowing of eyes or skin (in advanced cases)
However, these symptoms are non-specific and easily overlooked. In my experience, most diagnoses are made incidentally—patients come in for a routine checkup, and their blood tests reveal elevated liver enzymes, or an ultrasound shows fatty changes.
When symptoms do appear, they’re often due to inflammation in the liver (known as non-alcoholic steatohepatitis, or NASH). If left untreated, it can progress to fibrosis (scarring) and even cirrhosis—a stage where the damage becomes irreversible.
I always advise my patients: if you experience unexplained tiredness, loss of appetite, or dull abdominal discomfort, don’t ignore it. A simple blood test can tell us a lot about your liver’s condition, and early detection is the key to complete reversal.
How I Diagnose Fatty Liver in My Patients
When a patient visits my clinic with general complaints like fatigue, mild abdominal discomfort, or simply for a routine check-up, I often suggest a liver health evaluation. Most cases of fatty liver are discovered unintentionally through these regular health screenings. Diagnosing fatty liver requires a combination of clinical assessment, blood tests, and imaging. Let’s break down how I usually approach it.
Physical Examination and History Taking
The process starts with a detailed medical history. I ask about lifestyle habits—diet, alcohol intake, physical activity, family history, and other health conditions like diabetes or thyroid issues. Even small details matter, such as how often a person eats outside, their sleep schedule, and whether they’ve been gaining weight gradually.
During a physical exam, I check for signs like an enlarged liver (hepatomegaly), tenderness in the upper abdomen, and sometimes mild jaundice (in more advanced cases). In many people, however, the physical exam may appear normal despite significant fat accumulation in the liver—hence the need for further testing.
Blood Tests and Liver Enzymes
Next, we do blood tests, which are a crucial part of the diagnosis. I usually order liver function tests (LFTs) to measure enzymes like ALT (Alanine Aminotransferase) and AST (Aspartate Aminotransferase). Elevated levels of these enzymes suggest liver inflammation or damage.
Other important parameters include:
- GGT (Gamma-glutamyl transferase) – Often raised in fatty liver and alcohol-related damage
- Lipid profile – To check cholesterol and triglyceride levels
- Fasting blood sugar and HbA1c – To assess insulin resistance and diabetes risk
These results give a clearer picture of the liver’s metabolic health. However, blood tests alone can’t confirm fatty liver; they simply raise suspicion.
Ultrasound and Imaging Tests
To confirm the diagnosis, I recommend an ultrasound scan of the abdomen. It’s a simple, painless, and highly effective imaging test that can detect fat deposits in the liver. The ultrasound report might describe terms like “fatty infiltration” or “increased echogenicity,” which indicate excess fat buildup.
In more advanced or unclear cases, we may use FibroScan (liver elastography) to measure liver stiffness—helpful in detecting fibrosis or early cirrhosis. For very complex cases, MRI or CT scans provide detailed imaging, though these are not usually needed for initial diagnosis.
Sometimes, a liver biopsy (taking a small tissue sample) is done if we need to know the exact stage of damage, especially when we suspect NASH or cirrhosis. But thankfully, most patients can be diagnosed and managed without needing an invasive biopsy.
Stages of Fatty Liver Disease Explained
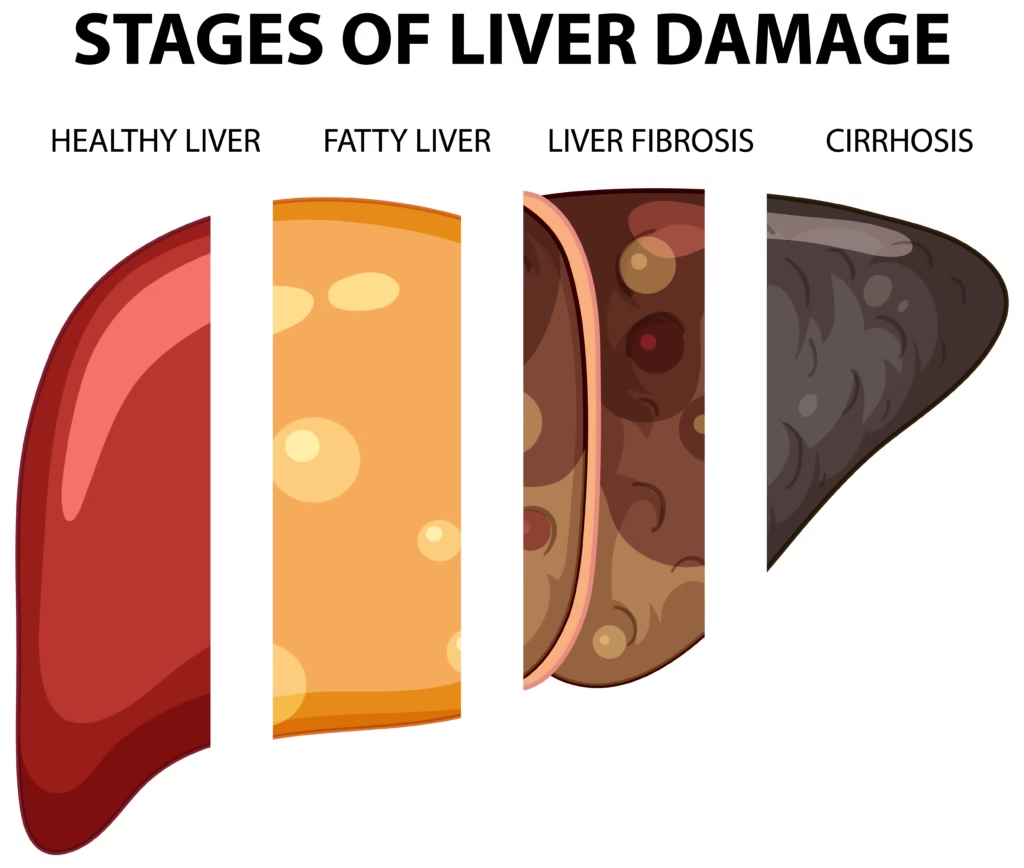
A lot of my patients often ask me, “Doctor, how serious is my fatty liver condition? Is it reversible?” To answer that, I explain the four main stages of fatty liver disease. Understanding where you stand helps set the right expectations for treatment and recovery.
- Simple Fatty Liver (Steatosis):
This is the earliest stage where fat accumulates in liver cells, but there’s minimal or no inflammation. Most people are asymptomatic here, and the liver function remains normal. The great news is—this stage is completely reversible with diet and lifestyle changes. - Non-Alcoholic Steatohepatitis (NASH):
When fat accumulation starts causing inflammation and liver cell injury, it progresses to NASH. Here, blood tests often show elevated liver enzymes. This stage requires immediate lifestyle modification to prevent further damage. - Fibrosis:
In this stage, ongoing inflammation leads to scarring (fibrosis). The liver still functions, but the damage begins to accumulate. The fibrosis may be mild, moderate, or severe, depending on how long the liver has been under stress. - Cirrhosis:
This is the final and most serious stage. The liver becomes hard and scarred, losing its ability to function properly. Cirrhosis can lead to complications like fluid buildup, jaundice, and even liver failure. At this point, the damage is irreversible, though progression can be slowed.
I always emphasize to patients that early diagnosis means the difference between complete recovery and permanent damage. The earlier we act, the more we can help the liver heal itself—it’s one of the most regenerative organs in the body.
Why You Shouldn’t Ignore Fatty Liver
It’s easy to brush off fatty liver as “no big deal,” especially when you’re not feeling sick. But that’s exactly what makes it dangerous. Fatty liver is a ticking time bomb if left untreated. Over time, simple fat accumulation can trigger chronic inflammation, leading to NASH, fibrosis, and ultimately, cirrhosis.
Moreover, fatty liver doesn’t just affect the liver—it’s linked to serious metabolic complications like diabetes, heart disease, and even certain cancers. Studies have shown that people with NAFLD have a higher risk of heart attacks and strokes, even if they don’t drink alcohol or smoke.
Another point patients often overlook is the connection between gut health and liver health. A diet high in processed food disrupts the gut microbiome, leading to inflammation that directly impacts the liver. This gut-liver connection means your digestive system’s health can either protect or harm your liver.
Ignoring fatty liver can also lead to fatigue, mental fog, poor metabolism, and difficulty losing weight. The liver plays a vital role in energy production, so when it’s burdened, your entire body feels it.
I tell my patients: “Your liver is your body’s silent engine. Take care of it before it stalls.” Luckily, the majority of cases can be reversed naturally—without medication—if addressed early.
How to Reverse Fatty Liver Naturally
Whenever I diagnose a patient with fatty liver, the first question they ask is, “Doctor, can it be reversed?” And my answer is always a confident yes—but only if you act now. The liver is one of the few organs in the body that can repair and regenerate itself, but it needs the right environment to do so. Reversal is not about taking a pill; it’s about creating daily habits that allow your liver to heal.
Let’s go through the key steps that I recommend to my patients for naturally reversing fatty liver.
Weight Loss and Lifestyle Changes
The single most effective way to reverse fatty liver is losing excess body weight. Even a modest reduction of 7–10% in body weight can significantly reduce liver fat and inflammation. But this isn’t about crash diets or starvation—it’s about sustainable, gradual changes.
Here’s what works best:
- Balanced Diet: Focus on whole, unprocessed foods.
- Portion Control: Eat slowly and stop when you’re about 80% full.
- Consistent Exercise: Aim for at least 150 minutes of moderate activity (like brisk walking or cycling) per week.
- Stay Hydrated: Drink plenty of water and limit sugary or carbonated beverages.
- Adequate Sleep: Poor sleep increases stress hormones and insulin resistance, both of which worsen liver fat.
I often encourage patients to make one small change at a time—switching to home-cooked meals, walking after dinner, or drinking more water. Over time, these habits build momentum and make healing sustainable.

Diet Modifications That Heal the Liver
The right diet can literally “cleanse” your liver from the inside out. I recommend what’s called the Mediterranean-style diet, which emphasizes:
- Fresh vegetables and fruits
- Whole grains like oats, brown rice, and quinoa
- Lean proteins
- Healthy fats from olive oil, nuts, and seeds
Avoid foods that cause insulin spikes and inflammation. That means cutting down on:
- Refined carbs (white bread, pastries, pasta)
- Sugary beverages and desserts
- Fried or fast food
- Processed meats like sausages and bacon
One practical tip I give patients is to replace sugar cravings with fruits. For example, if you crave something sweet after meals, have a small apple or a handful of berries instead of chocolate or dessert. Small swaps like this can make a huge difference.
Exercise and Physical Activity
If diet is the fuel, exercise is the ignition that helps burn off liver fat. The goal isn’t to run a marathon but to be consistent. Even light physical activity improves insulin sensitivity and metabolism.
Some of the most effective forms of exercise for reversing fatty liver include:
- Brisk Walking: 30–45 minutes daily works wonders for liver fat reduction.
- Strength Training: Building muscle helps your body burn fat even at rest.
- Yoga and Stretching: Reduces stress hormones that contribute to fat storage.
Patients often ask me, “What’s the best time to exercise?” My response is usually: it depends on how long you can maintain your commitment consistently. Morning, afternoon, or evening doesn’t matter as long as you move daily.

Foods to Eat and Avoid for Fatty Liver Reversal
One of the most common questions I get in my clinic is: “Doctor, what should I eat and what should I avoid?” Here’s a simple breakdown that I share with my patients.
| Foods to Eat | Why They Help |
|---|---|
| Leafy greens (spinach, kale) | Rich in antioxidants that protect liver cells |
| Fatty fish (salmon, sardines) | Contain omega-3 fatty acids that reduce inflammation |
| Oatmeal and whole grains | Improve insulin sensitivity |
| Olive oil and nuts | Provide healthy fats that lower cholesterol |
| Green tea | Contains catechins that support liver detox |
| Garlic and turmeric | Natural anti-inflammatory and liver-protective agents |
| Foods to Avoid | Why to Avoid |
|---|---|
| Sugary drinks (soda, energy drinks) | Cause insulin resistance and fat accumulation |
| Refined carbs (white bread, pasta) | Spike blood sugar and worsen liver fat |
| Processed foods and snacks | High in unhealthy fats and sodium |
| Alcohol | Directly damages liver cells |
| Red and processed meat | Increases inflammation and cholesterol |
When patients make these dietary adjustments, I often see improvements in their liver enzyme levels within 3–6 months. The key is consistency, not perfection. A single “cheat meal” won’t hurt, but repeated bad habits will.
The Role of Intermittent Fasting in Fatty Liver Recovery
In recent years, I’ve seen remarkable results in patients who adopt intermittent fasting (IF). It’s not about starvation; it’s about giving the liver a rest from constant digestion so it can focus on repair.
The most common and safe approach is the 16:8 method—fasting for 16 hours (including sleep) and eating during an 8-hour window. For example, you might eat between 10 AM and 6 PM and then fast until the next morning.
Benefits of intermittent fasting for fatty liver include:
- Reduced insulin resistance
- Decreased fat storage in the liver
- Better metabolism and appetite control
- Increased energy levels
However, IF isn’t for everyone. I always recommend starting gradually—maybe by skipping late-night snacks—and ensuring you stay hydrated during the fasting period. Patients with diabetes or low blood sugar issues should consult their doctor before starting.
Incorporating fasting even 3–4 times a week can help your body shift from “fat-storing mode” to “fat-burning mode,” aiding liver recovery.
Medications and Medical Treatments Available
While lifestyle modification remains the cornerstone of fatty liver treatment, some patients may require medical support—especially those with advanced stages like non-alcoholic steatohepatitis (NASH) or fibrosis. In my practice, I always prioritize non-drug interventions first. But when lab results show persistent liver enzyme elevation despite lifestyle changes, it’s time to discuss medical management.
Currently, there’s no single “magic pill” to cure fatty liver. However, certain medications can support liver health and address underlying causes:
- Insulin Sensitizers (e.g., Metformin):
These help reduce insulin resistance and improve glucose metabolism. While primarily used in diabetes, they often benefit patients with NAFLD too. - Vitamin E Supplements:
Vitamin E acts as a powerful antioxidant, helping to reduce liver inflammation and oxidative stress. I prescribe it cautiously, especially for non-diabetic adults with biopsy-proven NASH. - Statins:
For patients with high cholesterol or triglycerides, statins can be useful. Despite the myth that they harm the liver, when used under supervision, they actually protect it by reducing fat buildup. - Omega-3 Fatty Acids:
Found in fish oil supplements, these help lower triglycerides and may improve liver fat content. - Pioglitazone:
Another insulin-sensitizing drug that has shown promise in reversing NASH in certain patients. - L-Carnitine and Silymarin (Milk Thistle):
These natural supplements are often used to enhance liver detoxification and regeneration. I’ve seen several patients benefit from them when used alongside dietary changes. - Newer Treatments Under Research:
Researchers are exploring drugs that target inflammation, fibrosis, and metabolism. While not yet widely available, they represent hope for patients with advanced disease.
Even if medications are prescribed, I emphasize that no drug can replace healthy living. Pills may support your liver, but only your daily habits can heal it.
Can Fatty Liver Return After Being Reversed?
This is one of the most important—and frequently asked—questions in my clinic. The answer is yes, fatty liver can come back if the underlying lifestyle causes aren’t corrected. Think of the liver like a sponge: once you squeeze the fat out, it can fill up again if exposed to the same unhealthy environment.
Here’s what causes relapse:
- Returning to old eating habits (junk food, sugary drinks)
- Gaining back lost weight
- Skipping regular exercise
- Poor sleep and unmanaged stress
- Excessive alcohol consumption
However, relapse is completely preventable. Once the liver has healed, maintaining good habits becomes much easier because your body feels lighter, more energetic, and balanced. I always tell patients that recovery isn’t a “diet phase”—it’s a lifestyle transformation.
To stay on track, I recommend:
- Annual liver function tests
- A liver ultrasound every 1–2 years
- Continuing with moderate exercise
- Eating a balanced, whole-food diet
- Managing stress through meditation, yoga, or hobbies
Your liver will reward you for consistency. Patients who stay mindful of their choices rarely see a recurrence, even years after reversal.
Tips I Give My Patients to Maintain a Healthy Liver
After years of practice, I’ve noticed a pattern among patients who successfully reverse fatty liver and stay healthy long-term. They don’t just follow rules—they build sustainable routines. Here are my top practical tips that I share with every patient:
- Eat Your Last Meal Early:
Try to finish dinner at least 3 hours before bedtime. This gives your liver time to rest and process nutrients efficiently. - Start Your Day with Warm Water and Lemon:
It’s a simple way to hydrate and gently stimulate liver function. - Limit Sugar in All Forms:
Remember, sugar hides in sauces, dressings, and “healthy” drinks too. Always read labels. - Use Healthy Cooking Oils:
Replace refined oils with olive oil, avocado oil, or mustard oil. Avoid reheating oil multiple times. - Avoid Over-the-Counter Painkillers (Unless Prescribed):
Excessive use of acetaminophen (paracetamol) or NSAIDs can burden the liver. - Include Liver-Friendly Foods Daily:
Garlic, turmeric, beetroot, and green leafy vegetables help in natural detoxification. - Stay Active Beyond Exercise:
Use stairs, walk short distances, and avoid prolonged sitting—it all adds up. - Prioritize Sleep and Stress Relief:
Stress and lack of sleep trigger hormonal imbalances that worsen liver fat storage. - Regular Checkups:
Don’t wait for symptoms. Annual liver function tests can catch early changes before they become serious.
I often say, “Your liver doesn’t need detox juices; it needs consistent love and care.” By following these steps, you create a liver-friendly lifestyle that keeps you energetic and disease-free.
Conclusion: Hope and Healing for Fatty Liver Patients
Fatty liver disease has become one of the most common metabolic conditions today, especially among people who don’t consume alcohol. It’s a reflection of our modern lifestyle—stressful, sedentary, and filled with processed foods. But here’s the hopeful truth: your liver can heal itself.
Through small, consistent steps—healthy eating, regular exercise, weight management, and mindfulness—you can reverse fatty liver completely and prevent it from returning. Remember, this isn’t about restriction; it’s about balance and giving your body the care it deserves.
As a doctor, I’ve seen countless patients restore their liver health naturally, regain their energy, and transform their lives. The liver is resilient—it just needs a chance to breathe, recover, and renew.
Take that first step today. Your liver—and your future self—will thank you for it.
FAQs About Fatty Liver Disease
1. Can fatty liver cause pain?
Usually, no. Fatty liver is mostly painless, but some people feel a dull ache or heaviness in the upper right abdomen.
2. Is coffee good for fatty liver?
Yes! Studies show moderate coffee intake can protect the liver and reduce inflammation.
3. Can fatty liver lead to liver cancer?
In advanced stages (cirrhosis), the risk increases. That’s why early intervention is crucial.
4. Should I take liver detox supplements?
Not necessary for most people. Focus on whole foods, hydration, and good sleep—these are nature’s best detox tools.
Please don’t forget to leave a review.

I enjoyed reading this article. Thanks for sharing your insights.