Learn about cholelithiasis (gallstones) – causes, symptoms, diagnosis, treatment options, and prevention tips. Understand when gallstones need treatment and how to manage them effectively
Table of Contents
Introduction to Cholelithiasis
Definition and Overview
Cholelithiasis is the medical term for the formation of gallstones—solid deposits that develop inside the gallbladder. These stones vary in size from as tiny as a grain of sand to as large as a golf ball. Some people might carry gallstones without even knowing it, while others experience severe pain that can disrupt daily life. The gallbladder is a small but important organ in the digestive system.
Its main function is to store bile, a fluid that aids in the digestion of fats. When bile becomes imbalanced—containing too much cholesterol, bilirubin, or certain other substances—it can lead to the formation of crystals that eventually develop into gallstones. Over time, these stones may grow and cause blockages in the bile ducts, leading to inflammation and other complications.
Cholelithiasis is not rare—it affects millions worldwide, with higher prevalence in certain populations. Understanding this condition is essential because untreated gallstones can lead to serious problems, such as infection or pancreatitis. It’s not just a medical term you might hear in passing—it’s a condition that could be quietly developing without obvious warning signs.
Importance of Understanding Gallstone Disease
Knowing the basics of cholelithiasis is more than just medical trivia—it’s a step toward prevention and early intervention. Gallstones can often be managed effectively if diagnosed early, but many people dismiss mild abdominal discomfort as indigestion or stress.
This delay in recognition can lead to more complicated and dangerous scenarios. Understanding risk factors, early warning signs, and treatment options empowers individuals to make informed choices about their health.
Furthermore, gallstones are influenced by lifestyle, diet, and genetics, meaning you have some degree of control over your risk. For instance, certain eating habits can reduce the chances of gallstone formation, while poor choices can accelerate it. By being informed, you can take proactive measures, recognize symptoms before they worsen, and seek timely medical care.
Anatomy and Function of the Gallbladder
Location and Structure
The gallbladder is a small, pear-shaped organ located beneath the liver, nestled in the upper right portion of the abdomen. Despite its modest size—typically about 7–10 cm in length—it plays an outsized role in digestion. The gallbladder connects to the liver and small intestine via the bile ducts, forming part of the biliary tract. Structurally, it has three main parts:
- Fundus – the rounded, bottom portion.
- Body – the main storage chamber.
- Neck – the slender part of the gallbladder that joins it to the cystic duct.
Its walls are made of smooth muscle that contracts to push bile into the small intestine during digestion.
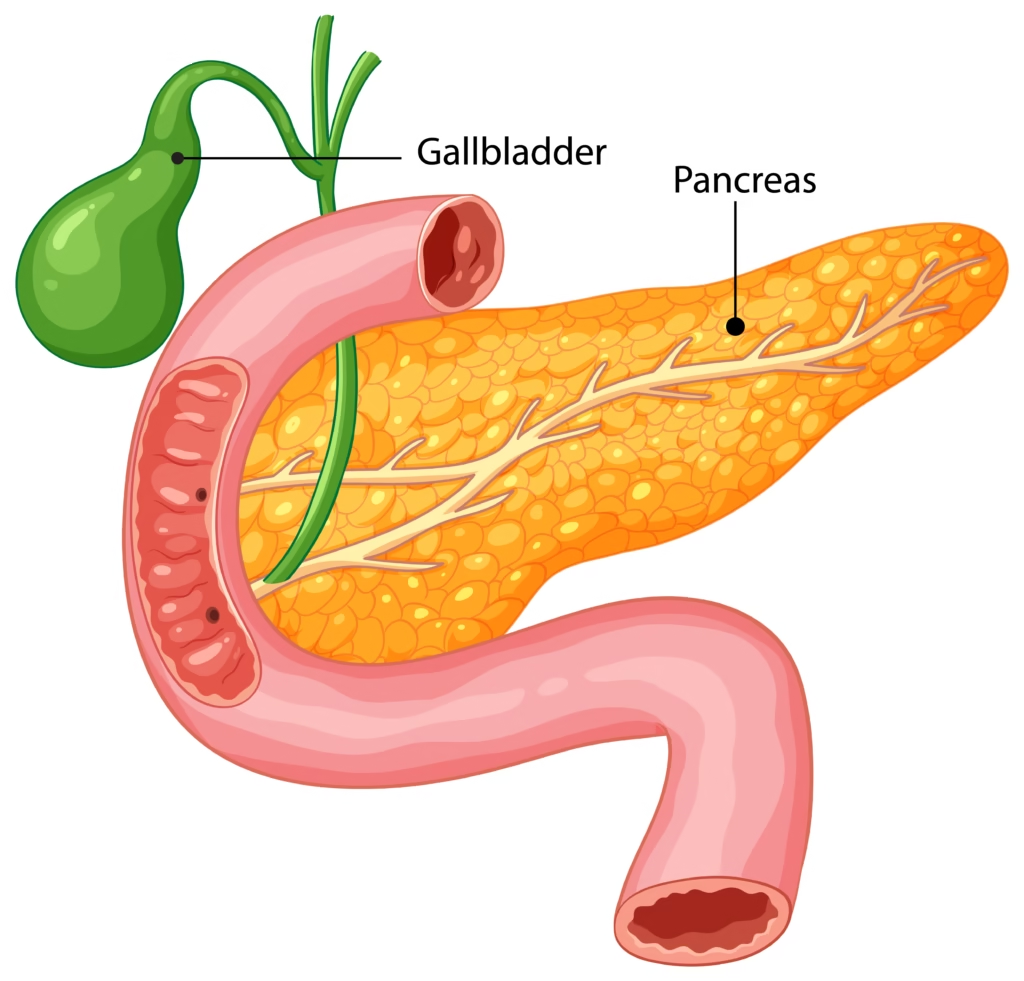
Role in Digestion and Bile Storage
The primary role of the gallbladder is to store and concentrate bile, a yellow-green fluid produced by the liver. Bile contains water, bile salts, cholesterol, and waste products like bilirubin. When you eat, especially fatty foods, the gallbladder releases bile into the small intestine to help emulsify and digest fats.
Without a functioning gallbladder, digestion is still possible—bile flows directly from the liver to the intestine—but fat digestion may become less efficient. This is why gallstone blockages can be so painful: they disrupt the flow of bile, leading to inflammation and digestive discomfort.
Types of Gallstones
Cholesterol Stones
These are the most common type, accounting for up to 80% of gallstones in Western countries.Gallstones develop when bile has an excess of cholesterol and an insufficient amount of bile salts to keep it properly dissolved. Over time, cholesterol crystallizes and grows into stones. Cholesterol stones are often yellow-green and can form silently for years before causing symptoms.
Pigment Stones
Pigment stones are usually smaller and darker in color, often brown or black. They form when there’s too much bilirubin in bile—a breakdown product of red blood cells. This can occur in conditions like liver cirrhosis, infections in the biliary tract, or certain blood disorders such as sickle cell anemia.
Mixed Stones
As the name suggests, mixed stones are a combination of cholesterol and pigment components. They are common and often linked to multiple risk factors. Mixed stones can form in people with both dietary and medical risk elements, making them more complex in origin.
Causes and Risk Factors of Cholelithiasis
Genetic Factors
Genetics plays a significant role in determining whether someone is prone to gallstones. If your parents or siblings have had gallstones, your chances of developing them are higher. Certain populations, like Native Americans and people of Hispanic descent, have genetic traits that increase cholesterol saturation in bile, making gallstones more likely.
Lifestyle and Dietary Habits
Your daily choices directly affect your gallbladder health. A diet high in saturated fats and refined carbohydrates increases cholesterol levels in bile, while a low-fiber diet slows digestion and bile movement. Rapid weight loss, crash diets, and prolonged fasting can also cause bile to become stagnant, promoting stone formation.
On the flip side, maintaining a balanced diet rich in fiber, healthy fats, and lean proteins supports healthy bile flow and reduces gallstone risk. Regular exercise improves digestion and prevents obesity—a key risk factor for gallstones.

Medical Conditions and Hormonal Influence
Certain medical conditions make gallstones more likely. Diabetes, liver disease, and metabolic syndrome all increase cholesterol and bilirubin levels in bile. Hormonal factors also play a big role—women are more prone to gallstones, especially during pregnancy or when taking estrogen-containing birth control or hormone replacement therapy. This happens because estrogen raises the cholesterol content in bile and also slows down the emptying of the gallbladder.
Symptoms and Complications
Common Symptoms of Gallstones
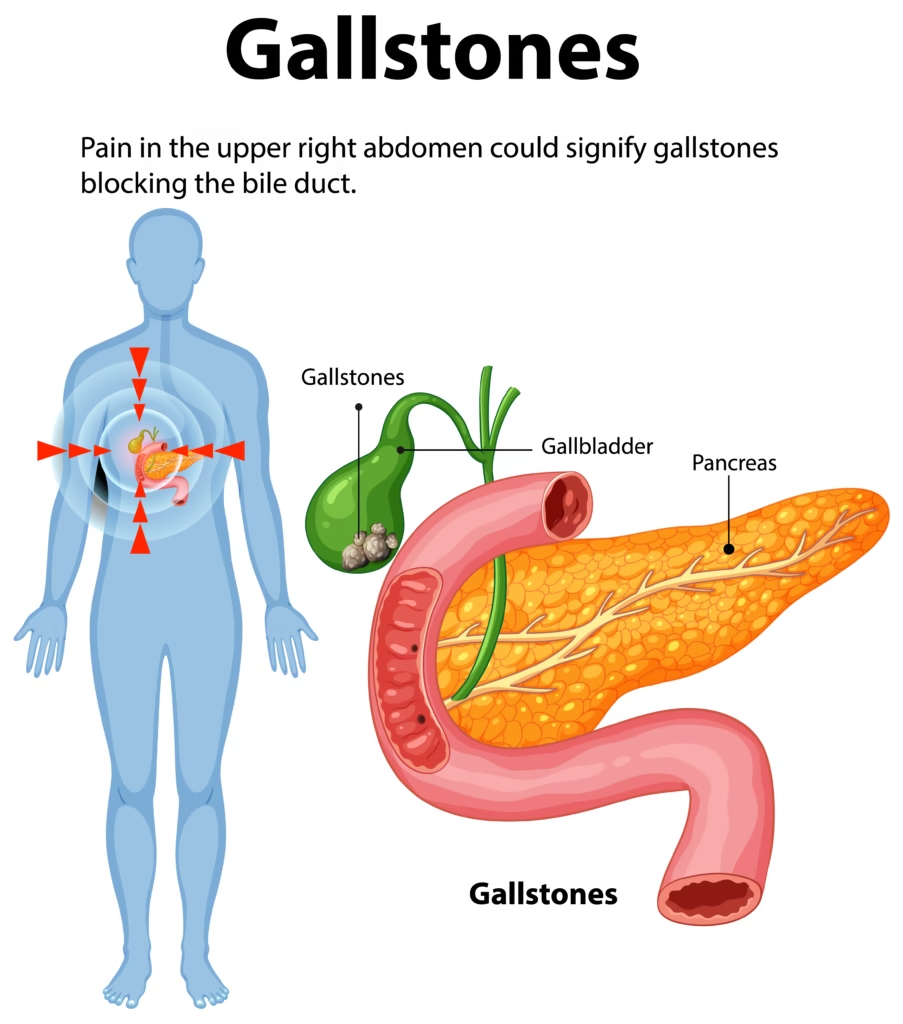
When gallstones cause symptoms, they often present as biliary colic—a sudden, intense pain in the upper right abdomen or under the right shoulder blade. The pain may last for a few minutes to several hours and is often triggered after eating a fatty meal. Other symptoms may include:
- Nausea and vomiting
- Indigestion and bloating
- Fever and chills (if infection develops)

Silent Gallstones
Interestingly, many people have gallstones without any symptoms—these are called “silent gallstones.” They’re often found accidentally during imaging tests for other issues. Silent gallstones usually don’t need any treatment unless they begin to cause symptoms or complications.
Potential Complications
If gallstones block the bile ducts, they can cause serious complications, including:
- Cholecystitis (inflammation of the gallbladder)
- Choledocholithiasis (stones in the common bile duct)
- Pancreatitis (inflammation of the pancreas)
Such complications may become life-threatening and need immediate medical care.
Diagnosis of Cholelithiasis
Physical Examination and Medical History
When a patient presents with symptoms suggestive of gallstones, a doctor begins with a thorough medical history and physical examination. They’ll ask about the nature of the pain—its location, intensity, duration, and triggers—as well as any digestive symptoms like nausea or bloating. They’ll also inquire about diet, family history, and any known medical conditions that may contribute to gallstone formation.
During the physical exam, the physician may perform a Murphy’s sign test, where they gently press under the right rib cage while the patient breathes in. If this causes sudden pain and stops the breath, it may indicate gallbladder inflammation. Though physical exams can raise suspicion, imaging is usually needed to confirm the diagnosis.
Imaging Tests
The most common and effective imaging test for gallstones is ultrasound. It’s quick, painless, and highly accurate at detecting stones and signs of inflammation. Other imaging options include:
- CT Scan – Offers detailed images of the abdomen and can detect complications.
- MRI with MRCP (Magnetic Resonance Cholangiopancreatography) – Provides detailed views of the bile ducts.
- Endoscopic Ultrasound (EUS) – Combines endoscopy and ultrasound for highly accurate detection of small stones.
Laboratory Tests
Blood tests can help identify complications of gallstones, such as infection or bile duct blockage. Doctors may check:
- Liver function tests – to detect bile flow obstruction.
- Amylase and lipase – to check for pancreatitis.
- White blood cell count – used to check for signs of infection or inflammation.
Treatment Options for Cholelithiasis
Watchful Waiting
If gallstones do not cause any symptoms, doctors often suggest a “watchful waiting” approach instead of immediate treatment. Many people live their entire lives without complications from these stones. The key is to monitor for any new symptoms and seek care promptly if they arise.
Medications
In select cases, gallstones can be dissolved using oral bile acid pills like ursodeoxycholic acid. However, this treatment works best for small cholesterol stones and requires months or even years to take effect. It’s generally used for people who cannot undergo surgery.
Surgical Removal (Cholecystectomy)
The most common and definitive treatment for symptomatic gallstones is gallbladder removal surgery. There are two main types:
- Laparoscopic cholecystectomy – a keyhole surgery done through small cuts using a camera. Recovery is usually fast, and most patients can return home the same day.
- Open cholecystectomy – Requires a larger incision, usually for complicated cases or when laparoscopic surgery isn’t possible.
Without the gallbladder, bile flows directly from the liver into the intestine. Most people adapt well to this change.
Non-Surgical Procedures
In rare cases, procedures like Endoscopic Retrograde Cholangiopancreatography (ERCP) are used to remove stones from bile ducts. This is often done in emergencies or when stones are stuck in the common bile duct.
Lifestyle and Dietary Management
Dietary Adjustments
A balanced diet can help both prevent and manage gallstones. Key dietary recommendations include:
- Increase fiber: Whole grains, vegetables, and fruits aid digestion.
- Healthy fats – choose options such as olive oil, nuts, and fish rather than saturated fats.
- Moderate calorie intake: Avoid extreme diets and rapid weight loss.
- Stay hydrated: Water helps keep bile fluid and reduces the chance of stone formation.
Regular Physical Activity
Exercise improves digestion, prevents obesity, and helps maintain healthy cholesterol levels—all of which lower gallstone risk. Even moderate activities like brisk walking, swimming, or cycling can be beneficial if done regularly.

Avoiding Risky Habits
Prolonged fasting, skipping meals, and high-fat binge eating can disrupt bile flow and promote stone formation. Maintaining a consistent eating schedule is a simple yet powerful preventive measure.
Prevention Strategies
Maintain a Healthy Weight
Obesity is a major risk factor for gallstones. Gradual weight loss of about 1–2 pounds per week can lower the risk, while crash diets and rapid weight loss should be avoided.
Balanced Diet for Long-Term Health
A Mediterranean-style diet, rich in vegetables, fruits, whole grains, lean proteins, and healthy fats, has been shown to lower the risk of gallstones and other digestive problems.
Manage Chronic Conditions
Conditions like diabetes, liver disease, and metabolic syndrome should be managed under medical supervision, as they increase gallstone risk.
Complications of Untreated Cholelithiasis
Cholecystitis (Gallbladder Inflammation)
When a gallstone blocks the cystic duct, bile builds up in the gallbladder, leading to inflammation. This condition, known as acute cholecystitis, can cause severe right upper abdominal pain, fever, and nausea. If untreated, it may lead to gangrene or rupture of the gallbladder—a life-threatening emergency.
Choledocholithiasis (Stones in the Common Bile Duct)
Gallstones can sometimes travel into the common bile duct, obstructing the flow of bile from the liver to the intestine. This blockage often causes jaundice (yellowing of the skin and eyes), dark urine, pale stools, and intense abdominal pain. It requires urgent medical intervention, usually through ERCP to remove the stone.
Gallstone Pancreatitis
When a gallstone gets stuck where the bile duct and pancreatic duct meet, it can cause inflammation of the pancreas, known as gallstone pancreatitis. This is a serious emergency that can lead to severe abdominal pain, vomiting, and very low blood pressure.
Gallbladder Cancer
Although rare, chronic gallstone irritation can increase the risk of gallbladder cancer. This type of cancer is aggressive and often detected late, which makes prevention through timely treatment important.
Gallstones in Special Populations
Pregnant Women
During pregnancy, hormonal changes raise the cholesterol levels in bile and slow down the emptying of the gallbladder. This makes pregnant women more prone to developing gallstones, especially in the second and third trimesters. While surgery is generally avoided during pregnancy unless absolutely necessary, careful monitoring and dietary adjustments can help manage symptoms until after delivery.
Elderly Patients
Gallstones are more common in older adults due to decreased gallbladder function over time. However, surgery in elderly patients carries higher risks due to other health conditions. Doctors often weigh the benefits and risks before recommending surgical intervention in this group.
Children and Adolescents
Though rare, gallstones can occur in younger populations—often linked to genetic conditions, obesity, or certain medications. Pediatric cases require specialized management tailored to age and overall health.
Prognosis and Recovery
Post-Surgery Outlook
Most people who have their gallbladder removed recover completely within a few weeks. Digestive adjustments are common but usually temporary. Eating smaller, more frequent meals and avoiding extremely fatty foods during recovery can ease symptoms.
Long-Term Health After Gallbladder Removal
Life without a gallbladder is generally normal. The liver continues to produce bile, but instead of being stored, it flows directly into the small intestine. Some people may experience mild diarrhea or bloating, especially after high-fat meals, but these issues typically improve with dietary changes.
Recent Research and Advances
Minimally Invasive Techniques
Laparoscopic cholecystectomy remains the gold standard for surgery, but robotic-assisted procedures are emerging, offering even greater precision.
Non-Invasive Stone Dissolution
Researchers are exploring more effective bile acid medications and even ultrasonic shockwave techniques to break down stones without surgery.
Predictive Risk Modeling
Advances in genetics and AI-driven diagnostics may soon allow doctors to predict gallstone risk earlier and personalize prevention strategies for high-risk individuals.
Conclusion
Cholelithiasis, though common, should not be underestimated. Gallstones can remain silent for years, but once they cause symptoms, the potential complications can be severe. Understanding the risk factors, recognizing early warning signs, and seeking prompt medical care can prevent serious outcomes. Lifestyle changes—such as maintaining a healthy weight, eating a balanced diet, and staying physically active—can go a long way in preventing gallstones. For those requiring treatment, modern surgical techniques offer quick recovery and excellent long-term outcomes. In short, knowing your gallbladder health could spare you a world of pain—literally.
FAQs
1. Can gallstones go away without treatment?
Small cholesterol stones may dissolve with medication, but most gallstones do not go away on their own.
2. Is surgery always required for gallstones?
No, surgery is only needed if stones cause symptoms or complications. Silent gallstones can often be managed without surgery.
3. Can diet alone prevent gallstones?
A healthy diet can significantly reduce the risk but may not prevent them entirely, especially if genetic factors are involved.
4. How long does recovery take after gallbladder removal?
Most people recover in 1–2 weeks after laparoscopic surgery, but complete adjustment may take a few months.
5. Can gallstones come back after surgery?
Once the gallbladder is removed, stones cannot form there again, but bile duct stones can still occur rarely.
Please don’t forget to leave a review.
